Medical School in the Age of AI: Grappling with the “Good Doctor” Conundrum
Medical School in the Age of AI: Grappling with the “Good Doctor” Conundrum

By Jan De Backer
The rapid rise of artificial intelligence (AI) is bound to cause a seismic shift in the professional landscape, challenging preconceived notions about the vulnerability of white-collar jobs to technological disruption.
Traditionally, the narrative has centered around the impact of automation and AI on blue-collar roles, with manual labor and repetitive tasks being supplanted by machines. However, this narrative is evolving, as AI begins to infiltrate domains that require higher cognitive functions, decision-making capabilities, and specialized knowledge. Nowhere is this shift more pronounced than in the field of medicine, a domain that has long epitomized the pinnacle of academic and professional achievement.
The practice of medicine and healthcare delivery is profoundly rooted in the individual knowledge and expertise of doctors and healthcare professionals.
Historically, becoming “a good doctor” necessitated many years of rigorous education and training, a journey characterized by its intellectual and financial demands. In countries like the United States, the pathway to a medical career is notoriously expensive, often saddling young doctors with substantial student loans—a burden that predicates the need for high future earnings. This paradigm, while designed to ensure a high standard of care, also reflects a system that is increasingly at odds with the potentialities ushered in by the age of AI.
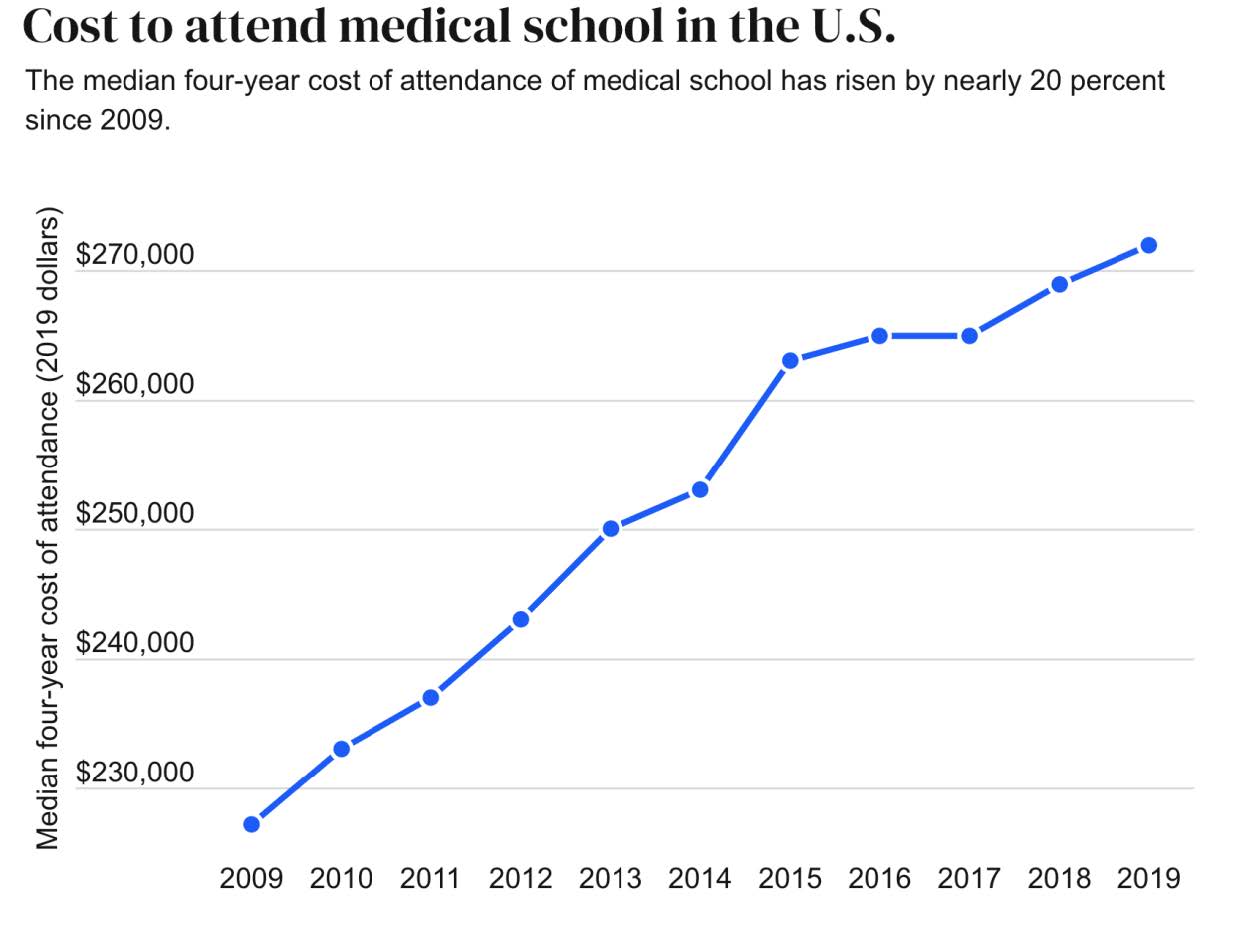
Source: Association of American Medical Colleges and Bankrate
The proliferation of AI and digital technologies has democratized access to knowledge, making it more readily available than ever before. While it is true that much of this information is unstructured and not immediately fit for medical application, there is a noticeable acceleration in the development of AI applications that are specifically tailored for healthcare. These technologies promise to streamline diagnostic processes, optimize treatment plans, and facilitate a level of personalized care previously unattainable through traditional means.
Looking forward, the implications of AI for medical practice are profound. It is conceivable that in the next decade, even the least academically distinguished doctor could prescribe nearly optimal treatments with the aid of generative AI technologies. This capability, while revolutionary and very good news for patients, underscores a pressing need to reconsider the structure and focus of medical education.
The case for reimagining medical school in the age of AI hinges on several key points. Firstly, the traditional model of medical education, with its emphasis on memorization and repetitive learning, may no longer be the most effective approach in an era where information is ubiquitous and constantly evolving. Instead, there is a compelling argument for reducing the
duration of medical education to align more closely with other professional degrees, such as those in law and engineering, which typically span 4-5 years. This revised curriculum would prioritize the development of skills in leveraging technology, interpreting complex data, and applying AI-driven insights in clinical settings.
Moreover, the doctor of the future must embody traits that technology cannot yet replicate — empathy, compassion, and exceptional interpersonal skills. The emphasis should shift towards nurturing these inherently human qualities, which are critical for patient care and cannot be substituted by AI anytime soon.
Despite the logical underpinnings of this evolutionary shift in medical education, significant barriers exist. The current generation of doctors, having invested over a decade into their education and training, may be reluctant to endorse a paradigm that ostensibly diminishes the value of their laborious journey. Additionally, medical schools and hospitals, which benefit financially from the existing system, may be reluctant to embrace change. The reduction in curriculum duration would likely impact revenue for medical schools, and hospitals might lose the inexpensive labor provided by interns and fellows.
Nevertheless, the momentum behind AI and technological innovation in healthcare is undeniable, and resistance to change may ultimately prove futile. The evolution of medical education is not just a matter of curricular adjustment but a profound paradigm shift towards a future where technology and human expertise converge to enhance patient care. As this wave of change approaches, it behooves all stakeholders in the healthcare ecosystem to prepare— whether by “grabbing a surfboard” or at least learning to swim.
The transition towards a more technologically integrated medical education system represents an opportunity to address longstanding issues within healthcare, including access, efficiency, and the personalization of care. By redefining what it means to be a doctor in the age of AI, we can pave the way for a healthcare system that is more responsive to the needs of patients and better equipped to meet the challenges of the 21st century. While the journey ahead may be fraught with challenges, the potential benefits for both healthcare providers and recipients are immense. As we stand on the cusp of this new era, the time is ripe for a bold reimagining of medical schools, one that embraces the transformative power of AI while reaffirming the irreplaceable value of human compassion and empathy in the art of healing.