Are we heading towards an iceberg in the field of respiratory medicine?
Are we heading towards an iceberg in the field of respiratory medicine?

By Jan De Backer
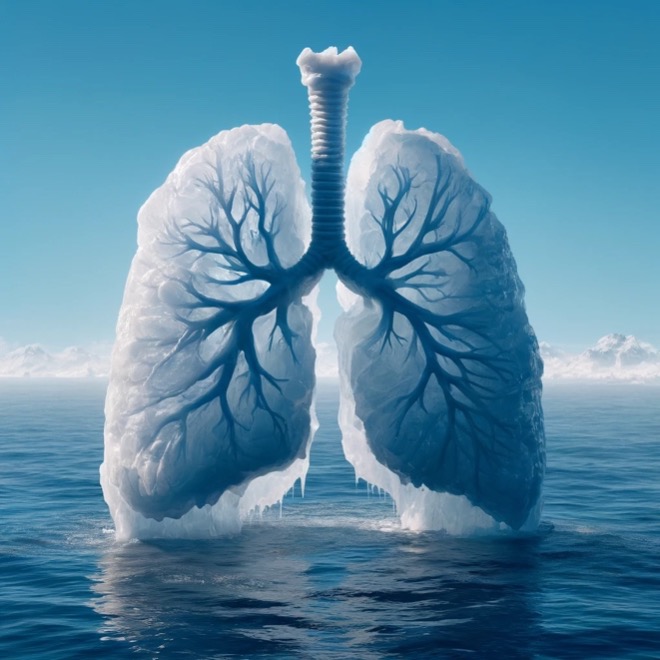 As the great Titanic set sail confidently into the North Atlantic, it was oblivious to the disastrous encounter that lay ahead. In a somewhat analogous fashion, the field of respiratory medicine in the United States is cruising towards a similarly unforeseen predicament—a shortage of specialists capable of navigating the treacherous waters of pulmonary diseases, including the rising tide of long Covid and other post-viral conditions.
As the great Titanic set sail confidently into the North Atlantic, it was oblivious to the disastrous encounter that lay ahead. In a somewhat analogous fashion, the field of respiratory medicine in the United States is cruising towards a similarly unforeseen predicament—a shortage of specialists capable of navigating the treacherous waters of pulmonary diseases, including the rising tide of long Covid and other post-viral conditions.
Let’s dive into the chilling numbers first. According to the American Medical Association, the count of pulmonologists took a nosedive from 5,263 active specialists in 2017 to 4,865 in 2021, a significant drop of 7.5%. More alarming, however, is the age distribution: In 2017, a full 88% of pulmonologists were older than 55. By 2021, this figure had climbed to a staggering 91%, marking the highest percentage for any therapeutic area by far.
What’s at the root of this decline? A considerable factor is the coupling of pulmonary training with critical care medicine. The latter is seemingly more attractive to incoming young doctors, with 76% of critical care specialists in 2021 being younger than 55 years. The allure? An attractive mix of action-packed responsibilities and a fatter paycheck.
The repercussions of a thinning frontline of respiratory experts are profound. With lung diseases on the rise, exacerbated by the relentless march of long Covid and its kind, the deficiency of dedicated professionals is a ticking time bomb. Even today, a lot of patients with respiratory complaints never see a pulmonologist, this trend is expected to worsen.
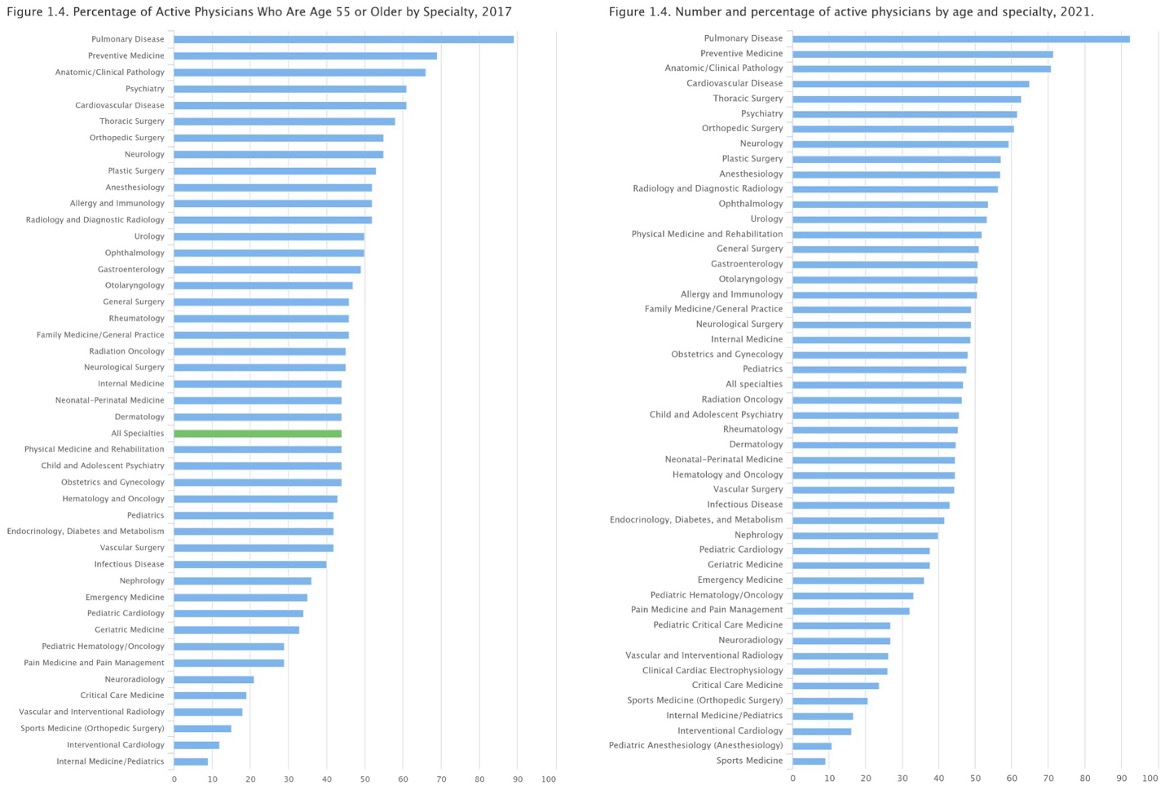
Figure 1: percentage of active physicians who are age 55 or older in 2017 (left) and 2021 (right) Source: AMA Physician Masterfile (December 2017 and 2021).
The solution must be multifaceted. To steer away from the iceberg, we should consider boosting the appeal of the pulmonology field. One tactic could be to increase the reimbursement rates, aligning financial incentives with the critical nature of the work. Moreover, embracing cutting-edge tools such as advanced imaging and artificial intelligence could not only streamline diagnostics and treatment plans but also pique the interest of a tech-savvy generation that’s eager to marry medicine with the miracles of modern technology.
There’s also a need to revamp the framework of pulmonary care. By weaving in rehabilitation and preventive measures as core components of patient care packages, the specialty can evolve from a purely responsive field to one that’s proactive and holistic. This strategic shift could position pulmonary medicine not just as a battle against disease, but as a champion of long-term wellness, an appealing prospect for the altruistic ambitions of many new doctors.
Moreover, it’s vital that we expand the ecosystem of care. Advanced nurse practitioners, respiratory therapists, and physical therapists must be empowered and trained to fill the widening gap. Engineers, too, can contribute significantly, particularly in refining non-invasive ventilation support systems, enhancing telemedicine capabilities and developing AI-based precision medicine tools. By fostering a collaborative environment that champions interdisciplinary contributions, the burden on pulmonologists can be eased, and patient care can be both enhanced and expedited.
Finally, there’s the innovative restructuring of care delivery. A network of outpatient clinics and mobile units could be the vanguard of respiratory care. These agile and accessible care points could deliver personalized, immediate attention, reducing the strain on traditional hospital settings and providing a timely response to patient needs.
This holistic strategy is not just an idealistic blueprint; it’s an essential course correction. As our population ages and the prevalence of respiratory diseases climbs, the shortage of pulmonologists is not a distant possibility—it’s an emerging crisis. And just as the fateful iceberg lay in the Titanic’s path, so too does this shortage loom over our healthcare system. It’s a challenge that requires immediate attention, innovative thinking, and collaborative action. We must heed the warning signs and adjust our course. The health of our nation—and the breath of millions—depends on it.